To successfully realize its reproductive function, the woman should carefully treat their own health. Permanent inflammatory processes in a small pelvis lead to serious malfunctions in the work and other organism systems. Therefore, you should not leave no attention to such pathology as chronic vaginitis, since without proper treatment, the disease can lead to severe consequences.
Description of the disease
Chronic vaginitis (colpit) is a common gynecological disease that can occur in a woman at any age. If you get into the mucous membrane of the vagina of pathogenic bacteria and their active reproduction, inflammation is developing, accompanied by itching and the appearance of discharge.
Sometimes the disease can immediately become chronic, for example, with an old or atrophic colpite.
Since during the remission, the signs of the disease are practically not manifested, the disease may exist for a long time (sometimes several months or years). It periodically exacerbates under the influence of external factors, for example, after ARVI or during pregnancy. On the general state of health, chronic colpit is not reflected, so women and do not rush to the doctor. With this course of the disease, infection is possible to penetrate the uterine pipes, the uterus, ovarian, which is capable of being the cause of infertility.
On the types, reasons, manifestations and treatment of collision - video
Where does Kolpiti be bored
- The chronic form of vaginite is a consequence of not fully cured acute inflammation. In some cases, the disease may initially flow hidden, which is characteristic of a variety of specific forms of collision.
- Long flow is typically for mixed vaginites, for example, bacterial-fungal, bacterial-trichomonaceous, etc.
- Chronic colpit often develops as a result of a decrease in immunity, provoked by the transfer of ORVI, chemotherapy, long-term admission of antibiotics. Therefore, a woman must be fully examined to eliminate the cause of the deterioration of the body's protective forces.
In addition, some factors increase the likelihood of chronic vaginite:
- supercooling;
- hormonal disorders;
- mechanical damage to the mucousa;
- neglect of personal hygiene rules;
- unprotected sexual acts.
Symptoms
In the chronic form of Coligation to replace exacerbations, periods of remission come. Recuses the disease most often with a decrease in immunity, excessive physical exertion, the effects of stress.
The disease is accompanied by:
- excretion of secretion with an unpleasant smell of various colors and densities;
- sensation of itching and burning;
- pulling pain at the bottom of the abdomen;
- discomfort during sex and urination.
Periodically, symptoms disappear independently. Therefore, women often do not pay attention to such manifestations, and this leads to the development of complications.In addition, there are specific features depending on the causative agent of the disease.
According to the selection, it is possible to determine the causative agent of the disease.
Signs of different forms of vaginitis - Table
Diagnostic methods
In case of suspicion of chronic colpit, the gynecologist appoints such studies:
- Inspection. During the study, the doctor assesses the condition of the mucous membrane, the presence of damage to the epithelium, edema, irritation. After examination, the gynecologist may assume some of the microorganisms provoked the development of pathology. In the chronic flow of the disease, there may not be a strong edema and abundant discharge, which makes it difficultdiagnostic.
- Colposcopy. Allows you to study the mucous membrane in more detail.
- Microscopic examination of smears. Chronic inflammation is characterized by an increase in leukocyte levels.
- Bacteriological sowing. The study allows you to determine the causative agent of the disease and its sensitivity to antibiotics.
- PCR. Used to determine infections that are transferred to the sexual way.
- Immunoenimative blood test. Allows you to identify antibodies to a specific pathogen, determine the duration of the course of the disease.
- Ultrasound. It is necessary when inflammation of inflammation on the internal genitals.
Non-specific chronic vaginites are developing under the influence of conditionally pathogenic microorganisms that are permanent in female genital organs. Usually the inflammatory process in such cases occurs when the immunity is reduced or a violation of the hormonal background. Therefore, it is necessary to take blood test for hormones and make an immunogram. Depending on the results obtained, the appropriate treatment of chronic collision is prescribed.
How to treat pathology?
Chronic specific vaginitis can be caused by one or several types of microorganisms. For the treatment of such a form of the disease, antiviral, antiseptic agents, antibiotics are used.
Sometimes it is very difficult to cope with Colpit, as many microorganisms can be hidden inside other pathogens. They are also capable of becoming resistant to the effects of used medicines. For example, chlamydia often live in trichomonads, so they are very difficult to destroy. In this case, first should be cured trichomonophone colpit, and then appointed antibiotics. But such therapy is not always effective due to the fact that the pathogens are able to quickly get used to antibacterial drugs. Therefore, the body "shake" with some medical products that activate the pathogen and sharpen the chronic process. And the disease in the acute stage is ease.
Systemic drugs with chronic nonspecific colpitis are not always needed.Typically, the treatment of notifying forms is carried out with the help of combined drugs of local action.
If chronic vaginitis arose against another pathology (diabetes mellitus, hormonal imbalance, etc.), it is primarily a treatment.
Preparations used in the treatment of chronic vaginite - Table
| Group of drugs | Name | Description |
| Antibacterial drugs |
| Required with a specific form of vaginite. Experate directly on the causative agent of the disease. It is first recommended to determine the sensitivity to antibiotics. |
| Antifungal drugs |
| Used with fungal infections. |
| Vaginal Candles or Tablets |
| Effective in bacterial and fungal infections, they have anti-inflammatory properties. They work directly in the focus of inflammation, facilitate the symptoms of the disease, carefully affecting the mucous membrane. |
| Hormonal agents |
| Used in the event that the disease occurred during menopause and is associated with a decrease in estrogen levels. |
| Vaginal creams and gels |
| Effective tools that do not affect the focus of inflammation. A positive effect is celebrated after the first application. |
| Probiotics |
| After the course of antibiotics, the reception of drugs restoring the vaginal microflora is required. |
Preparations for the treatment of chronic collision - gallery
Amoxiclav is used in the specific form of collision fluconazole needed during vaginites caused by fungus hexicone acts directly in the focus of inflammation  Climontore applies during menopause phenyatil eliminates inflammation and itching
Climontore applies during menopause phenyatil eliminates inflammation and itching  Lactonam restores the vagina microflora
Lactonam restores the vagina microflora
Folk treatments
Folk remedies can be applied as an addition to medication therapy, but only with the permission of the doctor. Many means based on healing herbs have antiseptic and anti-inflammatory properties, used for scrustling, irrigation irrigation.
To eliminate symptoms and acceleration of recovery, it is recommended to use such recipes:
- Infusion chiurela. The tool is chosen for sedentary baths by adding it to water. To prepare infusion:
- 2 tbsp. l. Dry cleanliness to place in the thermos and pour 1 liter of boiling water;
- soaking a few hours.
- Decrax of wildcroy, chamomile or calendula. Used as a solution for scrusts.
- 2 tbsp. l. the selected dry plant pour 0.5 liters of boiling water;
- three hours.
- Sea buckthorn oil. The tampon is soaked with this means and introduced into the vagina for the night. It is recommended to apply during the atrophic form of Coligation.
- Decoration of healing plants for douching. For its preparation you need:
- sage, Flowers Malva, Oak Crair and Chamomile Flowers in Equal Parts Mix;
- 2 tbsp. l. collection to pour 2 glasses of boiling water;
- soaking a few hours.
- Drawing by soda solution. Such treatment is effective with abundant discharge. To prepare the tool, 1 tbsp. l. Soda is dissolved in a liter of boiling water.
- Propolis with honey. The means soak the tampon and introduced into the vagina for 2 hours. The duration of treatment is 14 days. How to cook:
- take a piece of natural propolis (no longer than forest walnut), crushing;
- add 50 g of water, put on a water bath;
- after dissolving propolis, means to strain and cool;
- add 1 tsp. Honey.
Folk remedies from chronic collision - gallery
Cellular use for seats of field horsetail applied for douching sea buckthorn oil. It is recommended to use in atrophically colpidate of herbs decays the inflammation of the soda helps with abundant discolis removes inflammation
Diet
During the treatment of a chronic form of the disease, it is important to eat correctly. Woman should limit use:
- sharp, salty and fatty dishes;
- marinades and smoked;
- sweets and flour products;
- alcoholic beverages.
In the diet must be present fresh vegetables, fermented milk products, nuts, fruits, seafood.We will use the reception of special complexes of vitamins.
Consequences and complications
In the chronic flow of vaginitis, various complications may occur:
- Distribution of the inflammatory process to other small pelvis organs. At the started stage of the collision, cystitis, urethritis, endometritis, cervical erosion and other pathologies are possible.
- The chronic form of vaginite is very negatively reflected in the female reproductive health. The inflammatory process leads to the formation of adhesions in a small pelvis, the obstruction of the pipes, which makes it difficult to conceive. In addition, the risk of ectopic pregnancy, spontaneous abortion, premature genera, fetal infection increases.
- Girls can fire sex lips.
With adequate and timely treatment, complete recovery is possible. A woman must fulfill all the recommendations of the gynecologist and in the future do not forget about the prevention.
Prevention
You can avoid the development of the disease, adhering to some simple recommendations:
- any gynecological pathologies must be treated in a timely manner;
- comply with personal hygiene;
- refuse random sexual life;
- timely change underwear, hygienic agents;
- raise immunity, adhering to a healthy lifestyle and focusing correctly;
- do not use intimate hygiene tools that can irritate the mucous membrane;
- select only genuine underwear.
It is much easier to treat vaginitis in the acute stage, but if the disease has gained a chronic character, it is necessary to visit the gynecologist and to begin to combat this insidious pathology as soon as possible. Otherwise, not to avoid complications that are very dangerous for women's health.
Colpit - inflammation of the mucous membrane of the vagina.
Etiology Colport - more often infectious, caused by trichomonas, candom mushrooms, viruses of genital herpes, cytomegalovirus, mycoplasmas, ureaplasms, intestinal flora, patrogen pathogens (escherichia, protea, hemophilic vaginal stick, etc.).
Clinic Colpitis. For flow, 3 stages are distinguished: sharp, shadow, chronic.
Symptoms of Colport
With acute colpit, patients make complaints about the following symptoms: allocations (abundant, moderate, serous, purulent discharge); The feeling of gravity in the vagina region, sometimes at the bottom of the abdomen; itching, burning in the vagina region; Sometimes pain when urination.
In case of inspection using mirrors: pronounced hyperemia and the edema of the mucous membrane of the vagina; phetechial rash; Reddish nodules (infiltrates, pigment education epithelial cover); Erosion sections of the mucous membrane are possible.
In the subacute stage of the collision, clinical manifestations are expressed moderately (pain sneeze, the amount of discharge, the severity of hyperemia and edema of the mucosa decrease).
In the chronic stage of color, clinical manifestations are expressed slightly. The long-term flow is characterized by the presence of relapses. The main symptom is the separation of sexual ways of serous, sometimes purulent, often the feeling of itching is often arising.
Examination at Colpit
I. Objective examination:
Vi. Physiotherapy with Colpiti
Common contraindications for physiotherapy:
- malignant neoplasms;
- systemic blood diseases;
- sharp general exhaustion (cachexia);
- Hypertensive disease III degree;
- sharply pronounced atherosclerosis of brain vessels;
- heart disease in the decompensation stage;
- feverish states (an increase in body temperature above 38 ° C);
- Active Light tuberculosis;
- epilepsy with frequent seizures;
- psychosis with psychomotor excitation phenomena;
- peritonitis, abscesses;
- damage to the skin in the field of exposure.
I. Acute stage of Colport
1. The effect of an UHF electric field to the crotch area: 20-30 W, 10 minutes daily, course 5-8 procedures.
2. UV irradiation of vulva: 2 biodezes + 1 biolazosis in 2 days, course 6 procedures.
II. Tightening and chronic stage collision
1. Electrolyte moxibustion in conjunction with zinc electrophoresis on kellate: Current power 10 mA, 10 minutes, 1 time per week, course 6-8 procedures.
2. SMV therapy on the vagina area. Intensity 5 W (no more), daily, course 10-15 procedures.
3. UHF to the crotch area: 30 W, 20 minutes daily, course 10-15 procedures.
4. Local darsonvalization of the vagina: the power is average (to the sensation of light heat), 10-15 minutes, daily, course 12-15 procedures.
5. Laser irradiation of the vulva, contact method: 0.63 μm, PPE 10 W / cm2, 5-10 minutes daily, course 10 procedures.
6. Ultrafonophoresis of the vagina: a drug (Dimexide, sodium hydrocarbonate solution, ointment of the Rockortison guide), 3 MHz, 50-70 μm, 2-3 minutes daily, course 5 procedures
The use of ozone therapy in the treatment of non-specific collision and bacterial vaginosis.
Ozone has bactericidal, fungicidal, virologic, anti-stress, desensilizing and immuno-modulating properties. Ozone prevents microbial aggression (direct contact with microorganisms due to an increase in the oxidative potential destroys the capsid of bacteria and viruses and their DNA and RNA), activates the shield (increases the level of immunoglobulins).
Advantages of ozone therapy before antibiotics: Ozone does not negative effect on the body; It does not arise resistance; Ozone has a universal bactericidal action.
Ozonotherapy technique: ozone-oxygen gas mixture with ozone concentration 1500-2500 μg / l, obtained using osod / n / 0.1 ozone, series "Medasons" (Arzamas-n. Novgorod) are introduced into the vagina at a rate of 0.5-1 l / Min for 5-10 minute preliminary processing of the vagina in ozoneddistillated, daily, 1 rate is 5-8 days. The ozonation of distilled water is carried out immediately before the procedure using a saturable concentration of 5000 μg / l of the ozone-oxygen mixture, the duration of the ozonization of the vial of 400 ml of the bottle is 15 minutes.
Colpit (vaginite) is called inflammation of the mucous membrane of the vagina. This is a common disease with which most women at least once in their lives, but still faced. Colpitu is more susceptible to women of childbearing age, but the disease is also registered among representatives of the very young and elderly.
Causes of occurrence

Inflammation is the body's response to the aggressive impact of a certain factor: injury, chemicals, drugs, livelihoods of microorganisms, etc. Before talking about the causes and symptoms of the disease, it is necessary to determine the concept of normal vaginal microflora. Normally, the vaginal microflora is at about 95% represented by lactobacteriums (deterlene sticks) and representatives of the conditionally pathogenic flora (for example, genus candidate, staphylococcus, streptococcus, intestinal wand).
When influencing adverse factors (chronic diseases, endocrine pathology, decrease in immunity, treatment with antibiotics, etc.) changes in the microflora. The number of lactobacilli decreases, and this leads to a rapid propagation of the conditionally pathogenic microflora, the inflammatory process develops into the vagina.
There are also microorganisms causing sexually transmitted diseases (trichomonas, chlamydia, gonococcus, herpes virus). These are quite aggressive microorganisms, the ingress of which in the urinary organs even under the condition of normal microflora of the vagina will lead to the likely development of the inflammatory process.
Types of Colport

So, one of the reasons for the development of Coligation is microorganisms, namely: bacteria, viruses, mushrooms. Based on this, distinguish such types of collision:
- Specific;
- Nonspecific.
Specific colpitis is provoked by the pathogens of the STD - trichomonade, gonococcus, -virus. It is also worth remembering that girls vulvivaginit can be triggered by molds. Non-specific - conditionally pathogenic flora (staphylococcus, streptococcus, protemat, intestinal wand or mushrooms).
However, not only infection can cause the development of Coligation. So, there are still allergic and atrophic colpits. In the first case, the inflammatory process is a reaction to an allergen - a condom, lubricant, a drug introduced intrafined, foreign objects.

Atrophic colpitus develops with a violation of a hormonal background, namely a decrease in estrogen synthesis. Against the background of a reduced secretion of the hormone of the epithelium walls of the vagina, it is thinned, and the number of lactobacilli decreases. These conditions are sufficient so that with the minimum effects of the unfavorable factor, the inflammatory process is launched. Atrophic colpitus develops in women in menopause.
Symptoms of the disease
The severity of the clinical picture of the collision depends on the duration of the existence of the inflammatory process. Sharp counterpart proceeds expressed with symptoms delivering to a woman discomfort. These are symptoms like:
- The presence of mucous-purulent discharges with a smell of vagina;
- Itching and burning in the vagina and vulva;
- Strengthening painful sensations during sex, urination.
In the chronic form of the Coligation, these symptoms are little expressed, and sometimes the disease does not at all deliver a woman of any discomfort.
According to the characteristics of the selection, the doctor may suspect the causative agent of collision. For candidal collision, which is caused by a mushroom Candida, characterized by the appearance of blessed, curly discharge. In case of trichomonade, the collapse of the selection acquire a greenish tint, paradens, possess the characteristic smell of the fading fish. In the gonococcal, the excretion is acquired purulent character.

Complications
It's not so scolding to colpit, as its complications. All the danger is if the colpit is not treated, the infection is capable of spreading to other urinary organs. The infection spreads upwards, gradually involving in the inflammatory process of the neck of the uterus, the uterus itself, phallopievs pipes, ovaries. This is capable of violating the menstrual cycle, as well as problems with conception. In addition, infection is capable of spreading through the urethra and provoke the development of urethritis, cystitis. The presence of a long existing colusion can serve as a favorable background for the development of the erosy of the cervix.
Colpit is able to seriously complicate the course of pregnancy. The progression of infection can lead to its propagation on the oily water, premature childbirth. In addition, directly during childbirth during the passage of the generic paths the newborn can be infected with infection.
Diagnostics
 Often the complaints described by the patient are enough to ensure that the gynecologist suggested the presence of collision. But to confirm the alleged diagnosis it is necessary to conduct certain research. First of all, the doctor will definitely hold a gynecological examination. The introduction of a gynecological mirror in the vagina causes a patient with a colpitus pain. When examining the mucous membrane, the doctor can detect its swelling, redness, the presence of purulent or serous raids.
Often the complaints described by the patient are enough to ensure that the gynecologist suggested the presence of collision. But to confirm the alleged diagnosis it is necessary to conduct certain research. First of all, the doctor will definitely hold a gynecological examination. The introduction of a gynecological mirror in the vagina causes a patient with a colpitus pain. When examining the mucous membrane, the doctor can detect its swelling, redness, the presence of purulent or serous raids.
After a gynecological examination, a bacterioscopic and bacteriological study of the smear of the vagina and the urethra are carried out. This is necessary to identify the pathogen and the selection of the most effective therapy.
In a bacterioscopic study of the smear from the cervical canal, an increased amount of leukocytes is noted, the presence of bacteria, a stroke smear - 15-20 leukocytes in the field of view. To determine the causative agent of the Coligation, a bacteriological study of the discharge from the vagina is carried out.
Treatment
At the rate of treatment, sex contacts must be excluded. Since often Colpitis is a manifestation of STDs, treatment must also go through a gender partner. The lack of symptoms of STDs in a man does not exclude their presence at all, because the infection can flow hidden.
Treatment should be general and local. The main task of treatment is the fight against the causative agent of infection. To do this, use the following groups of drugs:
- Antibacterial (azithromycin, doxycycline, tetracycline, cefaapexin);
- Antiprotozoic (metronidazole) - for the treatment of trichomonaceous collision;
- Antifungal (fluconazole, ketoconazole, nystatin) - for the treatment of candidal collision;
- Antiviral agents (acyclovir, interferon).
Dosage and duration of drug intake are set by a gynecologist.
For local treatment, intravaginal candles, tablets and ointments are prescribed. Among the most popular:

Preparations for local treatment have a comprehensive impact. They not only suppress the growth and activity of pathogenic microorganisms, but also have an anti-inflammatory effect. In addition, with collision, they also prescribe the vagina with a solution of chlorhexidine, mormistine, chlorophilipte two or three times a day. It is not worth a similar douching for more than three or four days, as this may prevent microflora recovery.
 After the ethiotropic treatment has been conducted to restore normal vaginal microflora, eubiotics are prescribed:
After the ethiotropic treatment has been conducted to restore normal vaginal microflora, eubiotics are prescribed:
- Lactobacterin;
- Vagilak;
- Bificol;
- Bifidumbacterin.
Eubiotics contribute to the restoration of the microflora and the acidity of the vagina.
Estrogens are assigned to eliminate atrophic collision.
Treatment with folk remedies
In the complex treatment of collision, vegetable can be used. They cannot be the only treatment, since they are not able to influence the infection pathogen. But at the same time, some vegetable agents have an anti-inflammatory effect, eliminate itching and contribute to more efficient restoration of the mucous membrane of the vagina.
For the treatment of Coligation, you can use a decoction of chamomile. For its cooking, you need to pour a tablespoon of chamomile colors in dishes and pour a liter of boiling water. After that, the dishes should be covered with a lid. When the infusion cools, it must be strain. The prepared decoction is used for douching in the morning and in the evening. Infusion infestas can also be prepared from coltsfoot, sage, juniper, calendula, turns.
Can be used and sea buckthorn oil. It is necessary to twist a gauze tampon, die into the oil, and then enter it into the vagina for several hours.
G. Valeria, Medical Observer
Colpit is a vaginal inflammatory disease, most often infectious nature. The name of the disease is formed from the Greek word Colpos, in the Latin language its analogue - Vagina. Concerning colpit is synonymous with vaginitis, in medical practice you can meet with any of these concepts.
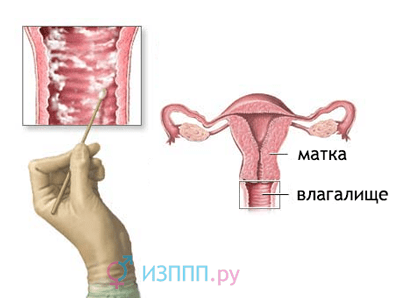
The vagina refers to the lower sexual paths and directly communicates with the external environment through its anticipation. The latter opens in the perineum between the small germ lips, so it is often moving into a colpit. The vagina is a hollow muscle body, the main function of which is the adoption of sperm during sexual intercourse. From the inside it is lined with a multi-layer epithelium - in strength it is similar to the skin epidermis, but its upper layer does not heal. It is thicker there are numerous glands that produce mucus to lubricate the vagina during intercourse and maintain comfortable conditions for normal microflora. Under the mucous membrane lies with a powerful muscular layer, built of cross-striped fibers. A woman can rapidly strain and relax them, and if desired and needed, to increase their strength by training (gymnastics for Kegel). The most outer layer of the vagina consists of dense connective tissue, which separates it from other organs of the small pelvis.

The structure of the female reproductive system
The vagina is directly connected with the uterus: in its wall "built-in" the narrowest part of the uterus is a cervix. The connection of the two organs is localized in the upper part of the vagina, and the space behind it is called vaginal arches. Break the front, side and backstore, the last is the deepest. It accumulates sperm after sexual intercourse and penetration of spermatozoa in the cervix.
Along the walls of the vagina are in a compressed state, and the front surface is pressed to the rear. The mucous membrane forms multiple folds. Such a structure allows the authority to stretch significantly during the sexual intercourse and the birth of the child. The vaginal epithelium has a close connection with the sex hormones and the composition of its cells varies depending on the stage of the cycle. Inside them there is a stock of carbohydrates in the form of glycogen grains, which serve as a nutritious substrate for the normal microflora of the vagina - lactobacilli or milk-sour chopsticks. Microorganisms are cleaved glycogen and synthesize the milk acid, so the acidic medium is maintained in the vagina, which deprivatives affecting the pathogenic and conditionally pathogenic microflora. In addition, lactobacillia produces hydrogen peroxide and substances with antibiotic activity. Any bacteria, accidentally falling into the vagina from the external environment, the rectum or with the penis of the partner die after a while they die and outward.
The number of glycogen grains in cells directly depends on the concentration of estrogen (female sex hormone) in the blood. In the first days of the cycle, the estrogen level is minimal, therefore the pH of the vagina shifts from acidic values \u200b\u200bto normal. During this period, the woman is most vulnerable to infection with STIs, since the inner medium of vagina becomes less aggressive for pathogens.
The maximum emission of estrogen into blood occurs during ovulation - on average 14 days from the beginning of the cycle (they consider from the 1st day of menstruation). The acidity of the vagina at this time is the maximum - pH reaches the values \u200b\u200bof 4-5, which is detailing for most representatives of pathogenic microflora. The risk of infection of STIs during this period is significantly reduced, so sex with a frozen partner does not always lead to the transfer of the pathogen.

pH level of vagina at different stages of women's life
The vagina has the ability of self-purification - the cells of its epithelium constantly listens and outlined with mucus into an external environment. Strengthening this process due to any cause leads to the formation of white - mucous drugs - in a noticeable amount. In the thickness of the mucous membrane, immune cells migrate capable of associating and neutralizing alien bacteria falling on it. They also secrete an IGA protective protein on its surface (immunoglobulin a), which destroys microbial bodies. Therefore, healthy women vaginitis is an extremely rare phenomenon, only aggressive pathogens of STIs are capable of calling it. Also the probability of its occurrence increases provoking factors:

All listed reasons negatively affect the state of the immune system, and therefore the general and local reduction in protective mechanisms occurs. The causative agents of the STIs and the nonspecific microflora get the opportunity to multiply on the surface of the mucous membrane and penetrate it.
Classification
There are several different criteria for which the separation of existing forms of disease in groups.
Depending on the cause of the vaginitis allocate:

By the duration of the flow distinguish:
- Acute - symptoms are preserved no more than 2 weeks;
- Subacutesth - up to 2 months;
- Chronic (recurrent) - Over 2 months.
By the nature of the lesion of the mucous membrane, the colpit can be:
- Diffuse - the entire inner surface of the vagina of the edema, hyperemic, mucous grainy, no raids;
- Serous-purulent - The mucous membrane is unevenly thickened, inflamed, separate areas are covered with a splip in the form of a white-gray film. The raid with difficulty is removed, leaves a bleeding ulcer.
On the path of penetration of infection, allocate:
- Primary vaginite - The causative agent falls from the outside immediately into the vagina;
- Secondary - Microorganisms penetrate with blood flow or lymphs from foci of other localization infection.
Symptoms
The clinical picture directly depends on the cause leading to the development of the disease.
Bacterial
Bacterial colpitis is different called "non-specific", since it causes its conditionally pathogenic bacteria living on the skin and in some cavities in normal. They are able to manifest their aggression only in the case of a decrease in immune protection or injury to the mucous membrane. Symptoms appear suddenly, it is often possible to trace the connection of the disease with the preceding sexual act. A woman is experiencing in the vagina, a feeling of cutting, heat in a small pelvis. become abundant, purulent, mucobist-purulentThey may have streams of blood in the erosive process on the mucous membrane. The smell varies from weak to pronounced rotten, they can be liquid, foamy. The big impurity of the pus and the raid epithelium gives the selections of a muddy white or yellow color, the consistency of them becomes thick.

Acute vaginite is often complicated. Inflammation easily passes to the overlying sections of the genital tract, and the flowing separations are irritated by the vulva, causing an agonizing itch. Woman combing outdoor genitals than aggravates the disease: additionally injures fabrics and enters new portions of the conditionally pathogenic microflora. Pain in the vagina can be moderate and strongly pronounced, sexual life during acute inflammation becomes impossible.
The general state rarely suffers, in some cases there is a moderate rise in temperature (up to 38 degrees C). The pathogenic microflora when entering the lymphatic vessels leads to an increase in the inguinal lymph nodes, sometimes they are inflamed. In the latter case, in the region of the groove bundle, with one or both sides, spherical formations of dense elastic consistency are observed to 1.5-2 cm in diameter sensitive during palpation, movable. As the symptoms of bacterial vaginitis, the size is normalized.
Candidose
The causative agent of the disease - the yeast fungus of Candida, which refers to a conditional pathogenic microflora and normally populates the skin, cavity, human mucous membranes. In the vagina, the microorganism gets from the rectum or with infected objects. The role of sexual transmission of Candida is small, as men rarely carry enough fungus for infection.

The disease begins sharply: There are burning, dryness, pronounced itch in the vagina. Often, the symptoms of the colusion are developing before menstruation or during it, after intensive sexual intercourse, antibiotic reception. In a few days appear curl sections from sex tract, They are white and have a sour smell. Such a characteristic symptom gave another name to candidal colpitu - thrush. Although, some forms of the disease proceed without such discharge, limited to painful itching in the region of vulva, intense pain and a feeling of burning in the vagina. This course of the disease is explained by the release of organic acid candidis cells as life products. They are annoyed by sensitive nervous endings, which are abundantly equipped with a lower third of the vagina. Permanent leather mass of the crotch and vulva leads to its thinning, substitution with connective tissue and to the loss of elasticity. The manifestations of the colusion are strengthened by the evening, especially after walking or physical activity. Often the allergic component in the form of elements is connected to the listed symptoms. cheeping red on the skin of vulva and crotch.
Candidose colpit easily passes into chronic shape and carriage, even against the background of treatment with antifungal drugs, especially if there is a diabetes or treatment with immunosuppressive drugs (cytostatics, glucocorticoids). In this case, it periodically recurns or manifests itself constantly, verses only during antifungal therapy.

The general condition of the woman does not suffer, the body temperature remains normal. The pronounced itching can break the dream and daily activities, but the symptoms of intoxication - headaches, the decline in appetite, the general weakness is not observed. Inguinal lymph nodes do not react or slightly increase in size.
Trichomonian
Trichomonade colpit is one of the most common sexually transmitted diseases. Causes his Trichomonadavaginalis, inhabitants in the urethre of infected men. Expanded infection occurs extremely rarely and is mainly due to the passage of the child by the generic paths of the mother, patient trichomonosis. Trichomonas - mobile microorganism, so easily penetrates from the vagina into the overlying genital paths, causing cervicitis, endometrite and urinary paths with development, cystitis. The causative agent reduces the activity of sperm both in men's and in female genital organs, so in the case of an asymptomatic course of infection, the main complaint of patients becomes infertility.
The incubation period of trichomonosis lasts from 5 to 15 days, at this time the pathogen is introduced into the mucous membrane and intensively multiplies. A sharp trichomonade colpit is manifested by pronounced itching, burning in the vagina, liquid foam discharge With an unpleasant smell. Often joined the symptoms of the injury of urinary tract -, painful, frequent urine release with small portions, but pain in the downturn area. The mucous membrane of the edema and painful, so sexual life is impossible during this period. Itching in some cases so pronounced that he breaks the night's sleep, the woman combs Vulva and crotch to blood. The reaction of the inguinal lymph nodes is missing or moderate, the general state is not violated.
Without proper treatment, Trichomonosis goes into a subacute, and then to the chronic stage. It can flow for a long time without symptoms, exacerbating during infectious diseases, pregnancy, reducing general immune protection. During remission, most women are marked and weak itching vulva.
Atrophic

Atrophic colpitus develops against the background of lack of female hormones - estrogen
Atrophic colpitus develops with a lack of female sex hormones - estrogen. It is preceded by menopause, an operation to remove one or both ovaries, the pitipofunction of the ovaries. In the cells of the epithelium sensitive to the hormonal background decreases the number of glycogen grains, which serve as a nutritious substrate for lactophilic bacteria. As a result, the amount of milky acidic sticks decreases, and the pH of the vagina shifts in a neutral side. There is a colonization of the mucous membrane of a nonspecific conditionally pathogenic microflora, which supports chronic inflammation in it. Along with the processed processes, the activity of the spun layer of the mucous membrane is reduced as a result of which it is thinning, loses its elasticity and becomes breaking.
The symptoms of Coligation develop gradually, starting with small dryness in the vagina, burning during intercourse, insufficient lubrication production. Scarest mucous membranes may appear milk and White Belie, slight itching vulva. Over time, signs of illness grow up, sexual life becomes impossible due to unpleasant sensations. Colpit is a chronic character with a hard flow, is not always amenable to therapy. The general condition of the woman is not broken, the body temperature remains normal, the inguinal lymph nodes do not react.
Video: Atrophic vaginitis, "Live Great"
Colpit during pregnancy
During the period of having a child, the hormonal background of women undergo serious changes: the amount of estrogen decreases, and the concentration of progesterone is growing. A yellow body hormone reduces the activity of the immune system to prevent its conflict with fetal proteins and prevent miscarriage. Therefore, most pregnant women can trace frequent episodes of respiratory infections, exacerbation of chronic inflammatory foci and joining vulvita, vulvovaginite. The relative deficiency of estrogen plays a certain role in the damage: the amount of glycogen in the cells of the epithelium decreases, the microflora instead of lactophilic becomes mixed.
Most often, the ticking in pregnancy is fungal character, and it flows quite hard: with a large number of secretions, pronounced swelling of the walls of the vagina, painful itching and painful pain in the perineum. Failure to comply with personal hygiene leads to a nonspecific vaginity, in this case, separated from the genital pathways with an unpleasant odor. It is easy to infect the trichomonade, as well as other sexual infections, so during pregnancy it is worth paying the significant attention of barrier contraception.

in collision during pregnancy it is worth using barrier congor
From the vagina, the pathogen easily penetrates through the neck into the uterine cavity and can lead to:
- Intrauterine infection of the fetus with the delay of its development, pneumonia, lesions of the skin and mucous membranes;
- Threat of abortion and miscarriage;
- Inflammation of placenta and fetoplacentage failure;
- Breaking the sex tract during childbirth;
- Sepsis.
Diagnostics
The diagnosis is set by a gynecologist during the collection of complaints, studying the history of the patient, inspection and according to the results of additional research methods. Different types of vaginite have a set of characteristic signs that can be judged by the cause of the disease.
Bacterial (nonspecific)
Complaints of the unpleasant discharge of a purulent nature prevail, often with blood admixture. Inspection in the mirrors during an acute stage is difficult: due to pain, the woman strains the muscles of the crotch and vagina, which prevents the introduction of the tool. Visually mucous bright red, edema, on its surface there are purulent overlays, point hemorrhages, gray-white films. The surface of it can be a grainy due to the towering elaborate papillas. Often the neck of the uterus is involved, the vagina is filled with inflammatory content that outlook.
The main method of diagnosis of vaginitis - microscopy smear
Microscopy plays the main role in the diagnosis of non-specific vaginitis. The method allows you to explore the species composition of the microflora of the vagina, to detect pathogenic microorganisms and assess their number. With a variety of staphylococci, streptococci, gram-negative sticks, dead cells of immunity - leukocytes, and a rapid epithelium. Lactobacilli is small, nonspecific microflora prevails.
Bakposev smear is rarely carried out due to its low informativeness. It is mainly used to quantify microorganisms of various types, their sensitivity to antibacterial drugs. The overall blood test becomes inflammatory only during the acute stage - the number of leukocytes increases, the number of young leukocytes increases, elaborates.
Candidose
The fungal colpit often has a relationship with treatment with antibiotics, diabetes, pregnancy in history. With the same frequency of women complain of the pronounced itching and characteristic selection of sex tract, usually these symptoms are manifested together. The introduction of the mirror in the vagina causes a moderate pain. In case of inspection, the edema is visible to the hyperemic mucosa, covered with a cotton chain in the form of an islands of an irregular shape with a size of 3-5 mm that do not merge among themselves. In the sharp stage, the flare is removed with difficulty, leaves a bleeding surface under him, when a disease transitions to chronic form, it is easy to remove it. The clinical picture is so characteristic that laboratory confirmation is usually not required. Difficulties arise with a long-term course of the disease, a lubricated clinic, the disappearance of the selection.

When studying the smear under the microscope, rounded Candida Tales are visible, interconnected into the chains. Plots of the raid consist of candida pseudomitia, broken cells of the epithelium and dead leukocytes. The smear is carried out to clarify the nature of the collision, since the method allows us to estimate the ratio of normal microflora, conditionally pathogenic bacteria and fungi. Along the way, the sensitivity of the causative agent to antifungal drugs is determined. In cases of severe disease, the disease with frequent recurrences is carried out by studying blood on antibodies to candida - they are found in high titer. Changes in general blood analysis are absent or nonspecific - the amount of eosinophils increases with an allergic reaction to the fungus, the ESO is accelerated.
Trichomonian
Trichomonad colpit from the groom can be suspected if it has a chronic urethritis chronic partner or after unprotected random sexual communications. The characteristic foamy type of discharge, involvement in the pathological process of urinary tract, cervix, bartoll glands and vulva also speak in favor of a trichomonaceous infection.
 In case of inspection in the mirrors, the mucule of the vagina is evenly hyperemic, edema, on it prominent dotted hemorrhages. Additionally, the bakposev smear, the material of which is taken from the urinary tract, vagina and vulva. In the native microscopy of native smear in the discharge, movable microbial calves are found, equipped with flagella or membrane.
In case of inspection in the mirrors, the mucule of the vagina is evenly hyperemic, edema, on it prominent dotted hemorrhages. Additionally, the bakposev smear, the material of which is taken from the urinary tract, vagina and vulva. In the native microscopy of native smear in the discharge, movable microbial calves are found, equipped with flagella or membrane.
Changes in the overall blood test appear during the acute stage - the number of leukocytes, immature forms of neutrophils increases, is increasing. Antibodies to trichomonade are found in the blood.
Atrophic
The diagnosis of atrophic collision does not represent difficulties, in contrast to its treatment. Anamnesis is clearly traced between the ovarian hypofunction or their removal and gradual development of the disease. In case of inspection, other signs of the lack of estrogen are identified: reduced skin elasticity, its increased fatness, enhanced hair loss on the head and excessive growth on the body. Inspection in the mirrors causes unpleasant sensations of burning, mucous vagina is hyperemic, thinned, multiple hemorrhages are often found on its surface. Options are missing either scanty. The doctor takes smear from the vagina and from the cervix to cytology - the study of the cellular composition to eliminate the malignant rebirth of the epithelium. Pathogenic microflora, as a rule, do not detect neither microscopy or method of bakposev. The number of lactobacilli is reduced, the proportion of conditionally pathogenic microflora increases.
General blood tests remain normal. To clarify the nature of the damage, the concentration of estrogen in the blood and its ratio with progesterone is determined.
Treatment
Treatment of Coligation is carried out in an outpatient basis, only women with severe purulent inflammation and pregnant women with a threat of miscarriage are hospitalized. Doctor's Tactics and Medicines Picks up with the main cause of the disease concomitant pathology and patient's condition.

In the sharp period of inflammation, the woman is shown by sexual rest, hypoallergenic diet with the exception of spices, smoked, marinades, citrus, chocolate. Supplements should be avoided, overheating, refuse to visit pairs, saunas, pool, not to take a bath. During menstruation, it is impossible to use hygienic tampons, and the gaskets change at least once every 4 hours. If the cause of the collision was the causative agent of the STI, the man partner must pass the course of antibiotic therapy even in the absence of the symptoms of the disease.
In case of bacterial, the target of the treatment is the rehabilitation of the vagina and the subsequent normalization of its microflora. For this purpose

To secure a positive effect, a course of polyvitamins are prescribed after the main course of treatment.
The fungal vaginite is important to treat in full at the acute stage and prevent its transition to a protracted flow. To this end, prescribe:
- Antifungal preparations of systemic effects - Fluconazole capsules 150 mg inside once;
- Local antimicotics in the form of candles, tablets, ointments - Pimafucin, Nystatin, Nitazol. Terezhin candles have antifungal, antimicrobial and anti-inflammatory effects, they are prescribed with expressed inflammation symptoms;
- Antihistamines to eliminate itching - Tueva, Supratine, Zoda;
- Immunomodulators to normalize the immune response - Timalin.

With trichomonade colpite, preparations are effective:
- System Action Antibiotics - Metronidazole, Facipin;
- Local treatment with antibacterial candles - clion d;
- Owl and sediment bath with antiseptics - potassium permanganate solution, chamomile decoction, calendula.
Treatment control is performed for 2-3 menstrual cycles. The absence of trichomonads in the smears taken after menstruation throughout this time speaks of the complete cure of a woman.
In atrophically, the doctor selects replacement hormone therapy In the form of estrogen-gestaggenic drugs for use inside (femoston) and locally (divigel). If necessary, correction of the microflora of the vagina with drugs of milk-acid bacteria (vagilac, acylac) is carried out.
L.
handiculate Colpit during pregnancy, preferably by local drugs, safe for the child - Hexicon, Terezhin, Nystatin. The need for other preparations determines the obstetrician-gynecologist, evaluating the severity of inflammation and the microflora of the vagina.
Video: doctor about Colpit (Vaginit)
Colpit (vaginitis) is the most common gynecological pathology. Most often, the disease is diagnosed in women of fertile age, but can develop in young girls and during menopause. Colpit is capable of rapidly progress, provoking the spread of infection on the rising ways.
In the absence of qualified medical care in a woman, after some time, endometrite or adnexitis is found, as well as serious problems with conception and having tooling the child. Independent treatment will not lead to the desired result due to the infectious nature of pathology. Before treating Colpit, a gynecologist will conduct a number of laboratory research to identify the species affiliation of the causative agent of the disease.
Basic principles of treatment
Pathogenic yeast fungi, pathogenic bacteria and viruses can become causative agents. During laboratory studies, not only the type of infectious agent, but also its sensitivity to pharmacological preparations is established. Most of the pathogens of the vaginite have developed sustainability even to modern wide range antibiotics, therefore an integrated approach to the treatment of collision in women is practiced. The following therapeutic techniques are used:
- the use of drugs for systemic and local treatment;
- conducting physiotherapy procedures;
- compliance with diet;
- strengthening immunity;
- restoration of the vaginal microflora.
The reasons for the development of the Coligation are most often endocrine disorders, venereal infections, non-compliance with intimate hygiene rules. If the colpit is triggered by diabetes mellitus formed by malignant tumors, thyroid diseases, then simultaneous treatment of the underlying disease is carried out. The most effective will be the treatment of vaginitis at the remission of these diseases. When patient with diabetes is neglecting the reception of antidiabetic agents or the correct introduction of insulin, then the colpit is rapidly progressing. The reason for this is the high level of glucose in the systemic bloodstream.
An important meaning for fast and effective therapy of vaginites of any genesis has an appeal to the doctor at the first signs of pathology. Self-treatment, as a rule, leads only to strengthening symptoms: discharge from the vagina, pulling pain at thenime of the abdomen, clinical manifestations of general intoxication. At home it is impossible to establish the type of pathogen, correctly pick up and apply drugs:
- antimicotic with fungal pathologies;
- antiviral in herpetic disease;
- antimicrobial and antibiotics in bacterial infections.
Daily and one-time doses of drugs, as well as the duration of the therapeutic course appoints a doctor. It takes into account the age of the patient, the degree of tissue damage, the presence of a history of liver diseases, the organs of the cardiovascular or urinary system.
During the treatment of the colusion, it should be launched at least three times a day with funds for intimate hygiene.
Colpit is good to treat, especially if the woman listens to the advice of the attending physician. Not only a quick recovery depends on this, but also a prevention of re-infection. What recommended gynecologists, urologists, venereologists to their patients:
- During the treatment of collision, regardless of the type of infectious pathogen, the sexual contacts should be completely stopped. The reason for such a ban is not only uncomfortable and painful sensations as a result of irritation of the mucous membranes of the vagina. Sexual contact will cause the advancement of pathogenic bacteria on rising paths. Also large is the likelihood of re-infection with colpitis of women, and with its specific infectious origin and men. In the diagnosis of venereal pathology, a sexual partner is treated.
- Collision therapy should be accompanied by a diet compliance to increase the efficiency of the pharmacological preparations used. It should be limited to the use of saline and acute products. If the patient's colpit is caused by pathogenic yeast fungi, then an indispensable condition for rapid recovery becomes a complete refusal of sweets and baking. In the diet, it is necessary to include as much fresh vegetables and fruits as possible.
- During the treatment of Coligation, intimate hygiene should be observed. The arms should be carried out at least three times a day, but during menstruation after changing the gaskets. When pathology is detected at a small girl, the genitals need to be washed after each emptying of the intestine or bladder. Doctors do not recommend using hygiene tools with fragrances or other additives.
- During the day, at least two liters of pure non-carbonated water should be used. The increase in urination contributes to the removal of infectious pathogens from the genitourinary system. Abundant drink helps to wash out the inflammatory foci of pathogenic bacteria and toxic products of their livelihoods.
Physiotherapeutic procedures
To speed up recovery and improve the efficiency of conservative therapy methods, physioproles are prescribed. They are not used in the acute flow of collision, but when chronic helped very well. Almost all physiothereders are painless and do not provoke any side effects. Gynecologists recommend to patients with these treatments due to the diverse impact on the body of a woman:
- reducing the severity of common and local symptoms;
- stopping the inflammatory process;
- increase the body's resistance to fungal, bacterial, viral infectious agents;
- improving the overall state of health;
- regeneration of damaged tissues.
To cure any colpitus will help the reception of pharmacological preparations and conducting physioturn sessions.
Their number varies depending on the severity of the clinical picture. In the therapy of bacterial and fungal vaginites, speed up the recovery will allow the application of the following techniques:
- ultraviolet irradiation with waves of small length;
- semi-posted with mangartee-acid potassium to replace infected areas;
- electrophoresis with zinc sulfate solution for the destruction of pathogenic fungi.
Intensive UHF therapy allows you to quickly stop inflammatory processes, prevent damage to the vaginal mucosa of infectious agents, reduce the activity of the mediators. Also, a woman is recommended to hold the following physiotherapy procedures:
- second-wave ultraviolet irradiation;
- thalassotherapy;
- air baths;
- laser blood irradiation;
- heliotherapy.
Such methods of physiotherapy do not affect the infectious agents directly. But after 5-10 sessions, the patient immunity is strengthened, as well as the general health condition.
Antibiotic therapy
This type of treatment is applied only in the diagnosis of chronic, difficult to therapy of colpits, or vaginites provoked by the gonococci. In the latter case, the prescription of the drugs of the cephalosporine series in the form of intramuscular infections is practiced:
- Ceftriaxone;
- Zefisim;
- Cefasoline.
And in the treatment of nonspecific chronic collision, protected semi-synthetic penicillins are used:
- Flemoclav;
- Panklav;
- Amoxiclav;
- Augmentin.
Conventional penicillins (amoxicillin, ampicillin, oplicsacin) are ineffective in vaginites, since the pathogenic bacteria has acquired resistance to their effects. Doctors prescribe antibacterial agents to patients, which include clavulanic acid. This chemical compound does not show any therapeutic activity, but has the ability to prolong and strengthen the effect of antibiotics. Clawulanic acid prevents the production of specific enzyme enzymes by bacteria, making microorganisms insensitive to drugs. When in force or the small efficiency of semi-synthetic penicillins, doctors replace them on macrolides - clarithromycin or azithromycin.

For dicks and baths in the treatment of collision, you can use infickers of healing herbs, such as calendulas
Sprinting
These procedures are very effective for external treatment of collision. The duration of such therapy is several days, until antimicrobial and antibacterial drugs of systemic and local action affect. They contribute to the destruction of causative agents of infection, which significantly reduces the severity of symptoms and the number of viruses, bacteria and fungi on the mucous membrane of the vagina. For douching, you can use such drugs:
- Chlorhexidine or its imported analogue of Mirisma;
- weakly pink potassium permanganate solution;
- Rivanol;
- Chlorophyllipt.
A solution of drinking soda has good antiseptic properties, especially if the candidial vaginitis occurs on the background of the abundant release of purulent white. For its preparation, 0.5 teaspoons of soda should be diluted in a glass of warm boiled water. For douching, infusions and champs of medicinal herbs are often used:
- sage;
- chamomile;
- calendulas;
- hypericum;
- nather.
To prepare the infusion, a liter of boiling water should be boiled. Spoons of dry vegetable raw materials and insist within an hour. After cooling and filtering, you can proceed to the procedure using a fringe. Such a local therapy method allows you to remove all pathogenic microorganisms from the vagina, prevent the damage to the mucous membrane to the toxic products of their livelihoods.
Treatment of atrophic pathology
The symptoms of atrophic collision suffer from a certain age category. As a rule, this type of vaginite is diagnosed in women after 50 years on the background of hormonal changes. The ovaries are terminated to fully produce estrogens, which causes climacteric manifestations - tides, emotional instability, headaches. One of the signs of natural menopause is thinning the mucous membrane of the vagina. It is easily injured, and fungi and bacteria are joined to the area of \u200b\u200bdamage. Hormonal pills and dragee are used as drugs and dragee, including vaginitis recurrences:
- Clair;
- Fermoston;
- Norcut;
- Duphaston;
- Angelica.

Vaginal PIMAFUCIN suppositories are used to treat robusts of fungal origin
The treatment of atrophic collision is to restore the mucous membrane of the vagina, eliminating the feeling of "dryness" and irritation. To do this, it is practiced to patients with vaginal candles or sheep cream with an active ingredient edging. The course of treatment is about two weeks, and then repeated as needed. Systemic replacement hormone therapy can last several years, which makes it possible to achieve maximum treatment efficacy. Not only menopausal symptoms disappear - the restoration of the mucous membrane of the vagina becomes excellent prevention of colpitis of any etiology.
Treatment during pregnancy
During the baby tooling, Colpit is developing more than 50% of women. In the role of provoking pathology of factors, a decrease in immunity and a change in the hormonal background are performed. The acidic medium of the vagina is gradually replaced by alkaline, and this serves as a favorable setting for the reproduction of pathogenic organisms. In some trimester, the vaginite is diagnosed, immediately proceeds to its treatment. Gynecological pathology can have a negative impact on the health of the mother, intrauterine growth and development of the child. How to treat colpit for pregnancy:
- Terezhinan is a combined antimicrobial, antifungal and antiseptic agent in the form of vaginal candles.
- Hexicon - the active ingredient of vaginal chlorhexidine suppositories violates the structure of the cell membrane of bacteria, contributing to the death of pathogenic microorganisms.
- Betadine - After the introduction of the candle, the vagina is released by the release of active iodine, which has a coagulating effect on microbial cells. Gynecologists prescribe this drug in early pregnancy to prevent damage to the thyroid gland of the child.
- Polizinaks - a combined means in the form of vaginal capsules is used in bacterial and fungal colpites. The drug can only be used in the last week of the child's nodding for the prescription of the doctor.
- Neo-Penotran - Vaginal suppositories exhibit antimicrobial, antifungal, antibacterial, antiprotozoic activity.
When diagnosing fungal vaginitis, Pimafucin, Clotrimazole, Nystatin is prescribed to a pregnant woman. Drying does not apply during pregnancy, but the use of seating baths will be very productive. The solutions of chlorhexidine, potassium permanganate, as well as infectios of medicinal herbs are suitable for washing the genuine organs, and mackelings. These procedures help to wash out the vagina of causative agents of collision and their growth and reproduction.
Systemic treatment
This type of therapy is almost always carried out at home and must be accompanied by dyeing, compliance with diet and intimate hygiene rules. Ethiotropic treatment is always directed to the destruction of the main cause of the gynecological disease - infectious pathogens. For this, drugs involve antimicotic, antiviral and antimicrobial activity. Often the woman is diagnosed with a mixed view of the vaginite. For example, in the absence of medical intervention, pathogenic bacteria are quickly attached to fungal colpitus:
- staphylococci;
- streptococci;
- intestinal wand.

In the treatment of colpits, a combination of drugs for internal and local use is applied
In order not to prescribe several diverse drugs at once, the doctor stops the choice on combined medicines of a wide range of action .. In order to make sure of the discharge from the vagina and pain at the bottom of the abdomen, the doctor may prescribe the following drugs:
- antimicotic - fluconazole, ketoconazole, itraconazole;
- antiviral - acyclovir, interferon;
- antimicrobials - trichopol, metronidazole.
An important part of the treatment of vaginitis of various genesis is the use of vaginal suppositories, balls, pills. They have a direct impact on pathogens formed inflammatory foci on the mucous membrane of the vagina. What drugs can prescribe the attending physician:
- Pimafucin;
- Clion d;
- Polizinaks;
- Hexicone;
- TERJIN;
- Nystatin;
- Clotrimazole;
- Caisten;
- Hynalgin.
The duration of the therapeutic course is from 10 to 14 days. Its duration depends on the species affiliation of the pathogen, the degree of damage to the mucous membrane of the vagina and the age of the patient.
Microflora restoration
If after etiotropic therapy in biological samples, the patient was not detected traces of infectious pathogens, the final stage of treatment was carried out. At this stage, women are prescribed drugs for the restoration of useful microflora in the vagina. Under the action of antibiotics and pathogenic microorganisms, lacto and bifidobacteria were killed. It is their livelihood products that created an acidic medium into the vagina, destructive for pathogenic fungi and bacteria. Vaginal suppositories are usually prescribed as eubiotics:
- Bifidumbacterin;
- Acilakt;
- Vagilak;
- Bificol.
The course of treatment is 5-10 days. At the recovery stage, patients also recommended receiving polyvitamins with trace elements, and in some cases immunomodulators.
Little girls and older women are sick vaginite. After the examination for all age categories, the doctor will make an effective therapeutic scheme individually for each patient. The earlier the gynecological disease will be diagnosed, the fewer consequences it will provoke.